As part of that process, I will be writing more blog posts. I got into biomechanics so I could do more math. I love math. Writing – not so much. It turns out, that in order to write a Master’s thesis…you have to actually write. Oops!
The benefit, however, is that I’m more comfortable writing now and better at explaining myself. I can only assume that the more I blog, the easier it will get – for me to accomplish and for you to understand.
Let’s start this journey with some basics on tissue mechancics, specifically Connective Tissues.
While I could write a book – wait a minute, I am writing a book – on the subject of tissue mechanics, I will introduce you here to some very basic, very generalized mechanical properties of connective tissues. Connective tissue is all over the body and does a lot more than it’s name reveals (connect things). Connective tissue shows up in the musculoskeletal system as fascia, ligaments, and tendons. It’s made of fibrous materials like collagen and elastin, plus some cells, some ground substances and proteins, lots and lots of water, and a bunch of other stuff that doesn’t apply to this particular post. It’s the collagen that we are going to talk about today.
Collagen is material that can be stretched. Like a really, really, really stiff rubber band. But like anything that can be stretched, it has a mechanical limit. If you stretch it within that limit, it behaves elastically – meaning it can return to it’s original shape. If you stretch it beyond that mechanical limit, it behaves plastically, meaning it will be permanently deformed. Permanently deformed equals damaged tissue. We don’t really want that do we? Stretch it even more and eventually, you will get total failure. Your rubber band will snap apart. We really don’t want that.
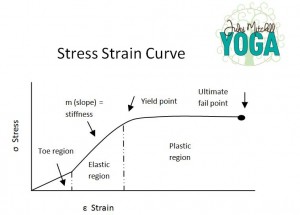
Visuals help, right? Here is a graph:
The vertical axis (y-axis for those of you who remember high school algebra) is the stress applied. That’s the nerdy way of say applied load or force. When you’re stretching, the applied stress is how much force is pulling on the tissue.
The horizontal axis is the strain – nerd speak for deformation.
Collagen fibers have a little crimp to them. Like when we crimped our hair in the 80’s. When you stretch the collagen, at first, the crimp straightens. That’s call the toe region. The collagen deforms a bit by getting longer and then the crimp returns when the load is removed.
Keep stretching (applying the load) and the tissue deforms a bit more. You’re still in the elastic region, the safe region. How much the collagen can deform is called yield. As long as you stretch below the yield point, you have not done tissue damage.
But stretch beyond the yield point and you have entered the plastic region. This when fibers begin to tear. Repairing these fibers is a slow process that can take up to 2-3 years. Tearing these fibers weakens the structural integrity of the tissues. That means it won’t do the best job holding you together that it can. If you keep applying that tensile load, the ultimate fail point is the end of the game.
Now this collagen is extremely strong and resilient material. It takes a lot of force to distend the tissue. So tearing your own connective tissue apart during a yoga pose, barring unforeseen accidents, isn’t too likely. However, entering the plastic region is not only possible, but depending on your genetics, also likely in certain yoga poses. Distend the tissue between 4% – 8% and you’re in the plastic region. That is not a typo. Four percent, 4%, is not a lot!!!!
Here’s the good news. Finally.
These collagen fibers are constantly remodeling and turning over. The cells are actually signaled to remodel the collagen based on the stretch they sense. Even the cells are little mechanical entities. Neat, huh?
Essentially, the properties of these connective tissues adapt to stretching loads. They will adjust their strength, stiffness (stiff is good in a biomechanical context), length, and yield points based on the stretching loads. As long as you don’t damage the collagen by distending the tissues into the plastic region. Repairing tissue damage is not the same as turnover and remodeling – the difference is something for another post.
In summary, stretch frequently and stretch without overloading. How do you do that? Stick with me, follow my blog, and all will be revealed in time. 🙂
PS. I post scientific articles and interesting research on my facebook page: www.facebook.com/JulesMitchellYogaBiomechanics